Comparing the Cost-Effectiveness of Alternative Policies for Recommending and Providing HIV Pre-exposure Prophylaxis to Men Who Have Sex With Men in the EU
Abstract
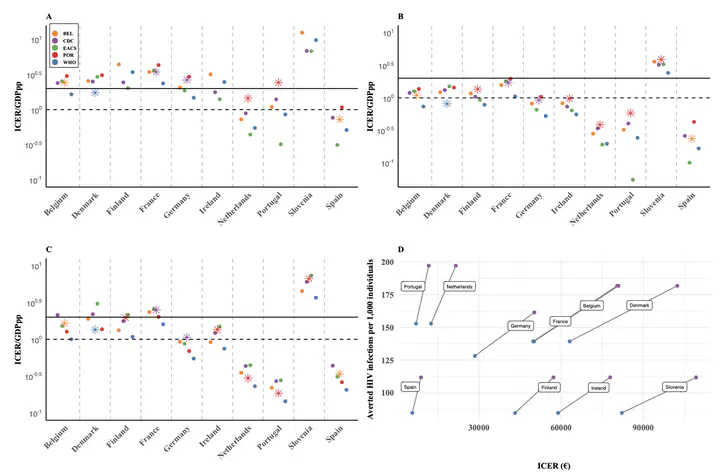
Background In the European Union, HIV disproportionately affects men who have sex with men (MSM), with prevalence rates ranging from 2.4% to 29%. Despite the high efficacy of pre-exposure prophylaxis (PrEP) in preventing HIV, its accessibility and uptake remain uneven across countries. This study examines the effectiveness and cost-effectiveness of different PrEP policies across 20 EU countries. Methods We employed a stochastic agent-based model of HIV transmission among MSM. The model incorporated data on sexual behavior, PrEP adherence and healthcare costs to evaluate the impact of five distinct PrEP eligibility policies. Outcomes included HIV infections averted, HIV-related deaths prevented, PrEP coverage, and incremental cost-effectiveness ratio. Findings Policies by the US CDC and Belgian authorities were the most effective in reducing HIV infections and deaths, driven by higher PrEP coverage. However, the WHO policy emerged as the most costeffective across the 20 countries, despite its current use being limited to Denmark. The European AIDS Clinical Society guidelines also showed potential, although not currently implemented. In countries without PrEP reimbursement, reducing drug costs would significantly expand the range of cost-effective policy options. Interpretation Optimizing PrEP policies is crucial for reducing HIV incidence among MSM in the EU. Broad eligibility criteria maximize effectiveness, while WHO guidelines offer a cost-effective alternative in constrained economic contexts. Our findings highlight the need for policy adjustments to enhance PrEP accessibility, inform national health strategies, and achieve sustainable HIV prevention across diverse settings.